Type 1 & the Big "M" - My Changing Basal Insulin Requirements
It is recognised that for women, hormones affect the management of type 1 diabetes at different stages of their lives – in adolescence, managing menstruation during the reproductive years, in pregnancy, peri-menopause and then menopause.
I went through adolescence at a stage in treatment when I couldn’t be very precise about identifying my body’s response. One injection a day and home urine testing gave no ability to closely monitor or respond to the turmoil that the changes in hormone levels caused.
With blood testing readily available by the time I was preparing and navigating my way through pregnancy, it was slightly easier to see the hormonal impact on my insulin requirements. I likened pregnancy with my son to climbing a set of stairs with very wide treads. My insulin dose requirements would increase at regular intervals as I progressed through pregnancy, then stabilise for a while before the next increase was required. Pregnancy with my daughter was a completely different experience – more like being in a washing machine. Insulin requirements and blood glucose responses were more variable.
Move on 10 to 12 years and a new kind of turmoil started to present itself. I eventually suspected that decreasing fertility levels, as I approached the next phase of my life, were causing increasingly variable blood glucose responses to situations that I thought I had found a way to manage.
Perhaps the most fascinating thing to see is how my overall background insulin requirements have been falling. Post pregnancy and breastfeeding, when hormone levels were once again more stable, I was on around 20 units of long acting insulin at bedtime. In my early 40s an increasing number of overnight and mid-morning hypos started a reduction in bedtime doses. After several years of experimenting with different brands of long acting insulin and reducing doses, I was finally approved for insulin pump therapy. I am pleased to report that this seemingly unavoidable pattern of hypos whilst on MDI has disappeared but it remains a challenge to find a basal rate that is a good fit. As I write, this continuing challenge has resulted in my doses now being almost half of what they were - I am currently on a total of 11.5u over a 24hour period. This has however been reduced to as little as 10u when undergoing extended episodes of overnight lows and increased to as much as 12.5u to deal with higher than desired overnight/early morning readings.
One of my great frustrations is being on the receiving end of the frequently offered advice concerning the importance of regularly testing basal patterns. The recommended advice to test if basal patterns are working is to conduct fasting tests on a regular basis, covering the different phases of the day. When testing, you want to be sure that the only thing affecting blood glucose levels will be the insulin so as well as avoiding food & pre-meal bolus doses, tests should not be conducted when exercising, undergoing major stress, when ill or when experiencing hormonal changes. Now my general feeling is that if you live a “normal” life and as T1s we are encouraged to live normal lives, how easy is it, regardless of your age or gender, to find a day that meets every one of those criteria. Then add in the perimenopausal logistics of having 23, 26, 28, 32 or 45 day cycles and fluctuating hormonal levels throughout those cycles that can cause several hours, half a day or several days of mayhem and finding a suitable time to test and a resulting basal pattern to use, becomes a nightmare.
I remember distinctly having my first longer than 28 day cycle. For days 29 to 35, insulin sensitivity seemed to increase again significantly and I had a run of days with hypos. The second time it happened some months later, I remember feeling smug and thinking, I know how to manage this based on my last experience. I cut basal rates expecting the greater sensitivity to return. Instead, I had a week of constantly battling higher blood glucose values. No matter how logically I approached situations, it was as if there was a gremlin turning everything on its head.
So after multiple attempts over several years of trying to test or even predict basal patterns, I became increasingly frustrated and gave up.
So what have I done to try to determine a basal rate to use? I had worked out that often the times I was more insensitive to insulin, when hormones were at play, seemed to be overnight and throughout the morning. The middle of the day tended to require fairly constant basal rates regardless of what was happening hormonally and then insensitivity might increase again slightly in the evening.
Three rough patterns
Firstly, I tried coming up with three very rough basal patterns, each one giving me between 1u and 1.5u more per day than the previous one and depending upon the sort of day or night I was having, I would choose the basal pattern to use. (These additional units tended to be spread over the night=time and early morning hours). I would regularly adjust my choice of pattern based on say the previous 12 or 24 hours of CGM readings. However, this caused huge mental turmoil. It is impossible to predict when hormones will impact and the blood glucose impact will never follow the same pattern. At bedtime, I would find myself sitting on the side of the bed looking at my blood glucose result, CGM trends and whether this had been as a result of hot flushes or night sweats the previous night. Add in normal considerations of what I ate for dinner, when I finished, whether a higher fat or protein content might impact blood glucose for longer, any likely “tail” from a bolus dose even if my pump reported no active insulin on board and I would tie myself up in knots. It can be very difficult knowing that you have an in range blood glucose reading at bedtime but then choosing a higher basal rate setting than “normal” because your overnight CGM trace from the previous night showed basal rates were too low. Overnight tonight they might be fine. I would choose one basal rate pattern and then find myself flipping between others and overwhelmed by indecision when the range of “what if” scenarios around nocturnal hypoglycemia entered my head.
Temporary basal rates
So why didn’t I just set a temporary basal rate? This is the favoured technique for dealing with illness but the difference here is that illness tends to last for an extended period of at least 24 hours up to several days with a more constant impact on elevating blood glucose levels. My experience is that any hormonal impact can last anywhere from several hours to several days but even over a period of several days may not have a continuous impact on sensitivities over a 24hour period.
A temporary basal rate is slow to take effect so could not be used on its own to deal with increased insulin insensitivity. A micro bolus would need to be used initially, to at least halt any rise to blood glucose levels, even if insufficient to return them to normal. If I then tried to combine a micro bolus correction with a temporary basal rate increase, I could often eventually “crash and hypo”. By the time the increased basal rate started to take effect, if the hormonal impact lasted only several hours, doses would be higher than needed and I would be left treating lows.
And finally? The other issue with a temporary basal rate was the pump alarm function. My pump vibrated every hour on the hour to remind me that a temporary rate was set and I didn’t particularly want this disturbance during the day and definitely not overnight.
Line of best fit
Returning to my memory of math lessons and scatter diagrams where we tried to plot a line of best fit, I decided to experiment with the same idea for setting a basal rate. I would not get hung up on trying to change between my three pre-set rates, even if I had several days of greater than usual variability, as chances were that no sooner would I change my settings than a new “normal” would present itself for another few days. Looking at CGM graphs for a week of results, I determined one basal pattern to keep to, that gave me a reasonable balance of blood glucose readings either side of a particular value I chose.
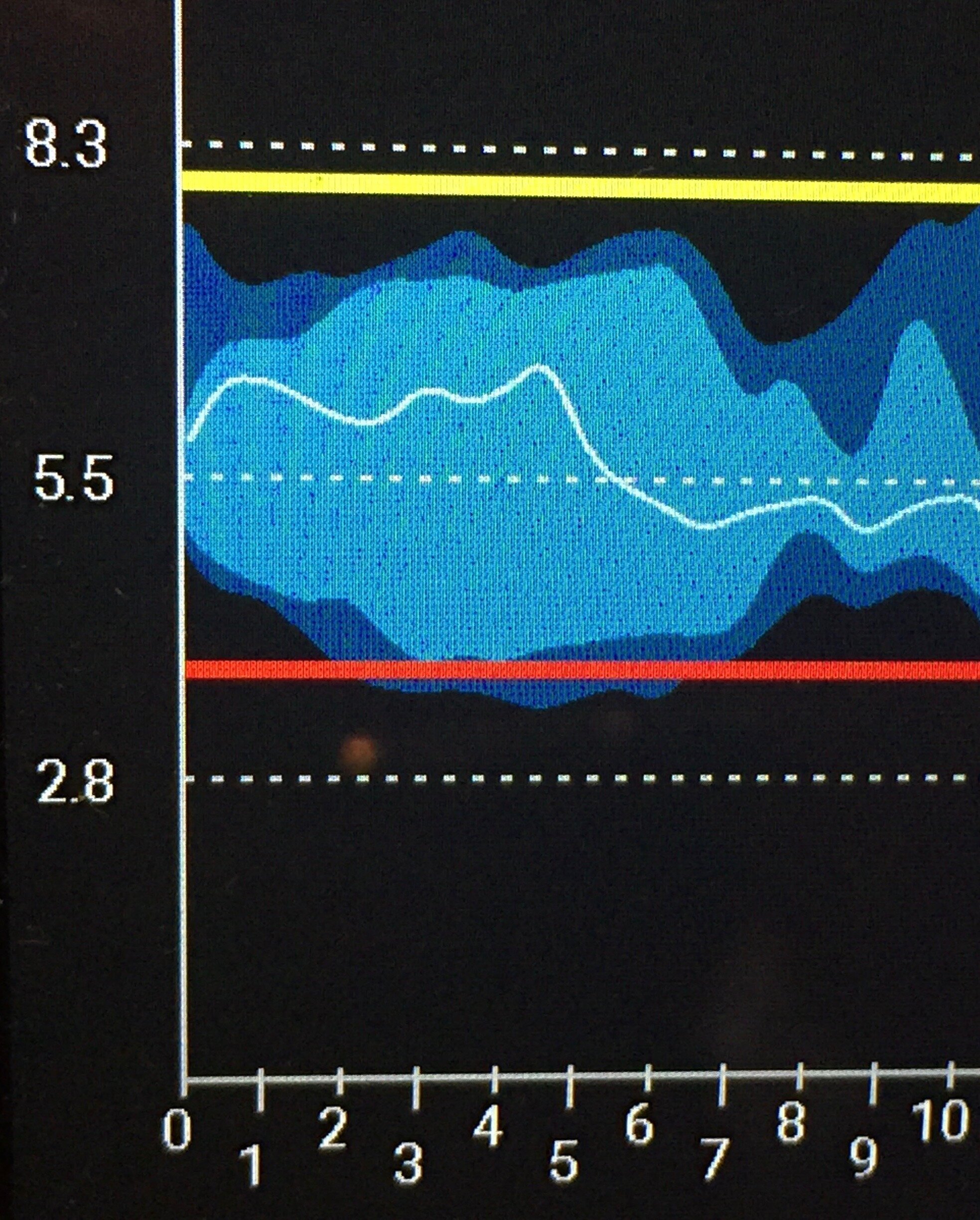
The graph shows a week of CGM results from overnight and into the morning, based on a basal rate of 11.15u over a 24hour period. The spread of readings shows that there is no obvious pattern to the dose required.
There were advantages to sticking to this one basal pattern. It limited the mental effort and difficulty in trying to second-guess the likely impact of hormones on my blood glucose results. However, that alone was not sufficient to keep readings within my upper and lower targets. In upper ranges I was topping up with micro-boluses and in lower ranges, I still had more low readings to contend with than I was happy about. The regular monitoring of my CGM and overnight alarms meant I was able to jump in to treat lows before they became serious but I was getting sick of the after taste from jelly babies and other high sugar hypo treatments.
Lowest basal rate
So I decided to try one basal rate but this time set it closer to the lower end of my range of options. I hoped that this would limit the frequency of treating minor lows but recognised instead that more micro-bolus corrections would be needed and would require equal care and patience in that when playing catch up and chasing increasing blood glucose levels, I would need to accept being slightly higher for longer and not over correct, resulting in eventual treatment yet again, of falling blood glucose levels.
For me, especially now in the latter stages of the peri-menopause, I find that this works reasonably well most of the time. (By most, that is a majority but still maybe only 60%). However, with a basal rate set closer to the lower end of the range of patterns I have needed, I do have to watch out for the extremes. There are still more days than I would like where I seem to revert to my pre peri-menopausal hormones and before I know what has hit me, am struggling to tame readings that may vary between 10 mmol/l and 15/16mmol/l at 8.30am, before eating any breakfast.
So if you are reading this hoping for answers, I’m not sure that I can offer any solutions, just a sharing of experiences. All methods tried have their pros and cons and none provide an ideal solution. I tend to move between the last two methods depending upon recent blood glucose behaviour and willingness to eat high sugar treatments for low blood glucose levels.
I hoped that once I could call myself fully menopausal (and that may only be three months away), the hormonal variations would start to reduce and it might start to become easier to identify one basal rate requiring fewer micro bolus adjustments over a 24hour period. I am beginning to doubt that, but only time will tell.
Disclaimer:
I am writing a series of blogs about my experiences of managing type 1 as I approach the menopause. I hope this will help others to understand the range of changes that may affect them. However, I am very aware that my experiences may well be very different to yours…. So please use this for ideas, discussion with HCPs and not as gospel. Please talk to your team before experimenting with techniques that have worked for me. Please experiment slowly and safely, to see how you react when trying to find techniques that may work for you. It has taken me nearly five years of self-funded CGM use and trial and error, to come up with my tool kit. Even then, it never works all of the time!