Type 1 & the Big "M" - Deconstructing a Hot Flush (Part 2)
I was lucky enough to have access to Dexcom G6 for several months in the autumn of 2018, as a result of volunteering for a research trial. I recorded details of my actions allowing a pictorial blog following the management of one particular hot flush on one particular night with type 1 diabetes.
This first graph shows my CGM readings for the preceding day. There were no extremes of blood glucose to blame for the overnight difficulties. (I will comment on the 10pm blip later in this blog). The “c” symbol identifies where I calibrated the CGM with a self-monitoring blood glucose (SMBG).
We started eating dinner at 7.30pm. As the majority of the meal was low to moderate glycemic index (GI) I injected only 5 to 10 minutes before eating. I ate:
Salad as a starter including lettuce, cucumber, tomato, artichokes, olives, grated carrot and goats cheese
2 slices of seeded wholemeal bread (estimated 40g C)
Grilled fish and green vegetables (no starchy carbohydrates)
Small round custard tart with raspberries (25g C)
One glass of red wine and water to drink
My usual insulin to carbohydrate ratio is 1u to 10g carbohydrate and as my blood glucose was in the normal range and I was expecting carbohydrates, based on my food choices, to be absorbed fairly steadily, I withheld 1u of my dose and decided to watch CGM trends before deciding if and when to add the final 1u of my expected usual dose.
My blood glucose response throughout the evening seemed to confirm my view of dosing for the food I was eating. Food was completely finished by 8.45pm.
For some reason, my CGM trace appeared to plummet just after 10pm. I hadn’t been low all evening, didn’t feel low then and did a SMBG to compare. At 22:16 my SMBG gave a reading of 4.2 mmol/l.
A difficult decision followed as to whether or not to calibrate. Given that the sudden drop was an odd response rather than the recognised lag of an accurate trace, I calibrated. The CGM cut readings for a while until it had sorted itself out.
Once back reading, the slope on my CGM trend line showed a steep rise. Using a further SMBG to confirm that this was tracking accurately after the earlier blip and knowing I was still 1u short on my normal evening meal insulin dose, I gave myself a 1u bolus. I also started to feel the early tell-tale signs of a hot flush.
As the hot flush symptoms became stronger, I gave a further 1u dose just after midnight to tackle what I knew would also be the start of an expected blood glucose climb from the flush. Although both doses were given less than 30 minutes apart, each was given to target a different issue. The first was targeting my food consumption (instead of using an extended wave bolus earlier in the evening) and the second was targeting the hot flush. Perhaps the 2u dose would be considered quite aggressive. It didn’t take long for it to turn around the blood glucose climb and show a CGM reading back in the normal range. However, flush symptoms were not abating and there was quite a rapid change of direction to the CGM trend again from 1am.
It is not unusual for the CGM trace to cut out with a rapid change in readings, whilst it tries to keep up. After about a one hour gap, I alarmed with a reading of 8.2 mmol/l. I decided, despite continuing to feel the full symptoms of the flush, not to add any further doses of insulin into the mix as the 2u had only been given just over 2 hours ago. However, my blood glucose levels continued to climb.
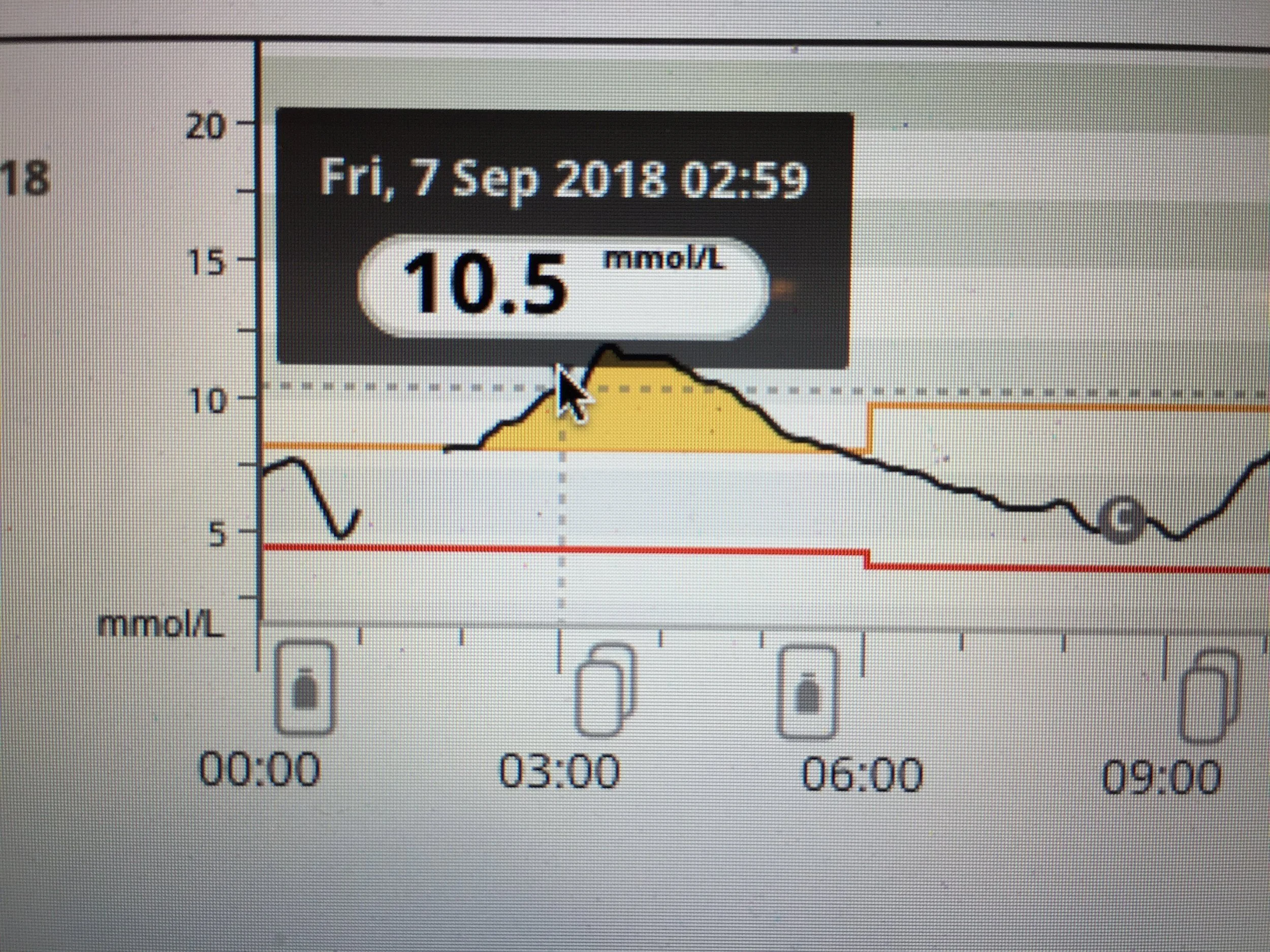
At 3am, almost 6.5 hours after finishing dinner and with a continuing upwards trend and CGM now reading 10.5 mmol/l, I wanted the spike to stop, I wanted the flushing to stop and I wanted to be able to sleep.
I gave a 2.5u bolus at 3.19am. Without hormones at play and using my insulin sensitivity factors, you would expect a dose of that level to drop my blood glucose to a level of 2 mmol/l. Instead, over the next two hours, my blood glucose increased to 11.3mmol/l (as you would expect with the insulin having to play catch up and the lead time it takes to work, whilst chasing the spike) before beginning to drop again almost two hours later to 9.2 mmol/l.
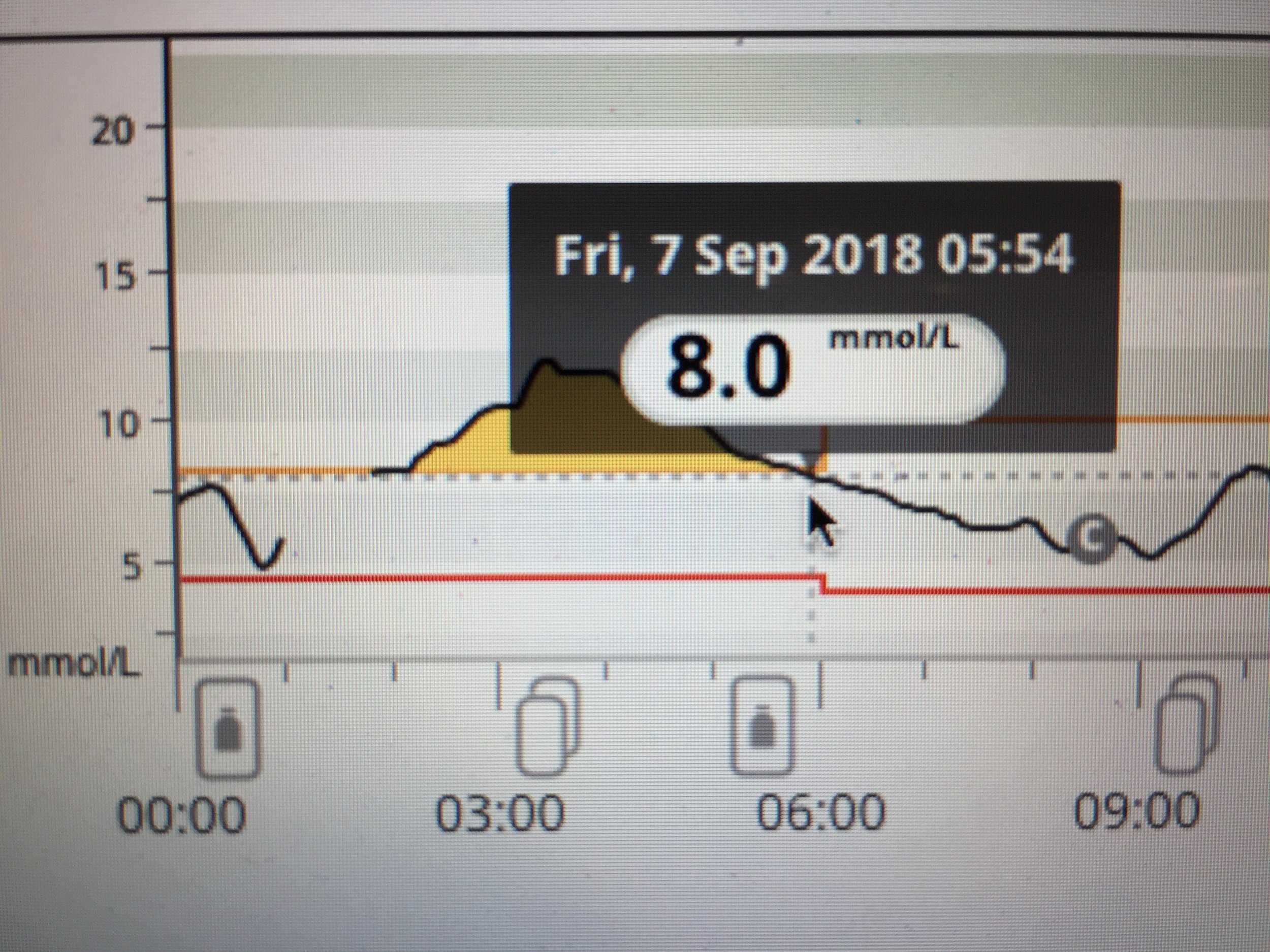
Although blood glucose trends were beginning to reduce by the early hours, I was still higher than I wanted and was still feeling the symptoms of the flush, so gave myself a further 1u dose almost 3 hours after the 2.5u correction.
My CGM trend shows that readings over the next two and a half hours were kept more stable by this additional 1u dose. A calibration on getting out of bed at 8.30am showed SMBG and CGM were showing very comparable readings of around 5.8 mmol/l.
So for a bad night of flushing, I gave myself an additional 4.5u of insulin between midnight and 6am. This excludes the delayed 1u given before midnight for carbohydrates at dinner. My usual insulin dosage between midnight and 6am could be anywhere from 2.85u to 3.15u if no flushes are occurring. So, I required more than double my usual total dose for the six hour period to return myself to a normal range.
Were there any delayed repercussions in doing so? Did I have bad hypos later in the day as a result of this additional insulin? The trend line for the following day is shown below and you can see - no hypos.